Introduction
Retinal vein occlusion (RVO) is the second most common retinal vascular disease to cause visual loss in adults after diabetic retinopathy. RVO has been classified into two main types, namely Central retinal vein occlusion (CRVO), Branch retinal vein occlusion (BRVO), the latter being more prevalent.
Hemi-retinal vein occlusion has been classified separately since pathogenetically they are different as compared to the above two groups. In the following chapter a brief introduction to these variants of RVO, along with their epidemiology, clinicopathological profile, and treatment has been discussed.
Epidemiology[1]
The most recently published study summarizing 68,751 individuals from 15 studies, quoted that the prevalence of RVO was 5.20 per 1000 (for any form of RVO). The prevalence of BRVO alone was 4.42 per 1000 (95% CI 3.65–5.19) and that of CRVO was 0.80 per 1000.
According to Hayreh et al, prevalence varied by ethnicity and increased with age, but do not differ by gender. The prevalence of CRVO is lower than BRVO in all ethnic populations and across all ages.
The probability of developing a second episode of occlusion in the fellow eye within the next 4 years was about 7%.
Demographic characteristics[1]
Distribution of various types of RVO:
Laterality:No significant difference between the affection of the two eyes.
Age and gender:Central retinal vein occlusion (CRVO) usually occurs in people >65 years of age, and the incidence is more in men as compared to women. Of all the CRVO, 71% were > 65 yrs.
Branch retinal vein occlusion (BRVO) also occurs primarily in people >65 years and does not have a sex preference. Of all the BRVO, 77% were > 65 yrs.
Prevalence:RVO though a disease of aged, does occur in young also. The incidence and prevalence in the young have not been studied.
Classification of different types of RVO [2]
Hayreh has described three primary types of RVO, each of which comprises two sub-types, making a total of six different forms of RVO.
Central Retinal Vein Occlusion (CRVO) is divided into two types:
- Non-ischemic
- Ischemic CRVO
These two forms have different pathogenesis, clinical features, prognosis and management.
Hemi-CRVO, like the CRVO, is of two types:
- Ischemic
- Non ischemic
Branch Retinal Vein Occlusion (BRVO) is divided, depending on which venous branch is affected, into two forms:
- Major BRVO
- Macular BRVO
Central Retinal Vein Occlusion
Pathogenesis[1-5]
Central retinal Vein Occlusion (CRVO): The exact pathogenesis of RVO still remains unclear but a few possible mechanisms causing CRVO enumerated include:
Occlusion of the vein by external compression by sclerotic adjacent structures (i.e.central retinal artery and fibrous tissue envelope) and secondary endothelial proliferation.
Occlusion by primary venous wall disease(degenerative or inflammatory in nature).
Hemodynamic disturbances produced by a variety of factors (e.g.,subendothelial atheromatous lesions in the central retinal artery, arterial spasm, sudden reduction of blood pressure, blood dyscrasias, etc and further aggravated by arteriosclerosis or unfavourable anatomic relations). Systemic risk factors associated with retinal vein occlusion are enlisted in Table-1 & some important thrombophilic disorder associated with retinal vein occlusion are enlisted in Table-2
The condition may arise due the individual cause or a combination of the above three. Systemic changes known as Virchow’s triad which includes: hemodynamic changes (venous stasis), degenerative changes of the vessel wall and blood hypercoagulability play an important role in pathogenesis. [3]
Hyperopia and glaucoma (22% IOP >22 mm of Hg) have been reported as local ophthalmic risk factors aggravating the underlying pathology in causing occlusion. [4]
There are differences in the role of each single risk factor in pathogenesis of CRVO and BRVO. For example, hypermetropia, arteriosclerosis and high blood pressure are more common in BRVO, whereas raised intraocular pressure is more common in CRVO. This demonstrates that CRVO and BRVO are different entities with different prognosis and management. [5]
|
Table 1.Systemic risk factors associated with retinal vein occlusion |
|
Hypertension, hyperlipidemia, diabetes mellitus |
|
Table 2.Most important thrombophilic disorders associated with retinal vein occlusion |
|
Anti-phospholipid syndrome (APS) |
Risk of CRVO decreases with-Increasing levels of physical activity, increasing levels of alcohol consumption, postmenopausal estrogens.
CRVO is classified into the two following types: [6]
Non-ischemic CRVO (also called venous stasis retinopathy)
This accounts for about 75% of all CRVO patients and is characterized by the appearance of areas of retinal ischemia smaller than 10 disc diameter area. The site of occlusion in this type is neither in the lamina cribrosa nor in the adjacent retrolaminar region but further back. The severity of retinopathy would depend on the site of occlusion - the farther back the occlusion, the milder the retinopathy, because of the availability of collateral channels.
Ischemic CRVO (also called haemorrhagic retinopathy)
Retinal ischemia larger than 10 disc diameter area is considered to be ischemic CRVO. The site of occlusion is most probably in the region of lamina cribrosa or immediately posterior to it. Senile degenerative changes in the wall of the CRV and adjacent central retinal artery results in marked narrowing of the lumen of the vein and sclerotic changes in the lamina cribrosa contribute to produce circulatory stasis and venous thrombosis. In patients with these predisposing changes, a fall of systemic blood pressure during sleep would finally complete the thrombotic process.
Non-ischemic CRVO changes to ischemic CRVO.: In>65 years old it is 13.2% at 6 months and 18.6% at 18 months whereas in age <65 years it is 6.7% and 8.1% respectively.
Cause:Blood flow in the retina depends upon perfusion pressure & further fall in perfusion pressure from marked nocturnal arterial hypotension would produce retinal ischemia during sleeping hours. The site of thrombosis in cases of non-ischaemic CRVO is farther back in the optic nerve. In few predisposed cases a gradual extension of the thrombotic process in CRV towards the optic disc up to or close to the lamina cribrosa can happen. This involves and thereby eliminates the available collaterals in the optic nerve (which previously protected these eyes) favoring the development of ischemic CRVO. [6]
Clinical Features
Nonischemic CRVO
May have no symptoms and it may be detected as an incidental finding on a routine ophthalmic examination.
The development of macular edema makes it symptomatic.
Visual symptoms if present, may be vague blurring of vision, frequently involving the central vision with an almost normal peripheral vision.
Amaurosis fugax occurs before the constant blur. A purple coloured blur is observed, particularly when non-ischemic CRVO is associated with cilioretinal artery occlusion.
Ischemic CRVO
There is always marked deterioration of vision
Noticed suddenly on waking in the morning. As in non-ischemic CRVO some patients may complain of episodes of amaurosis fugax before the constant visual blurring.
Presenting clinical findings are enumerated in the following table (Table-3)
|
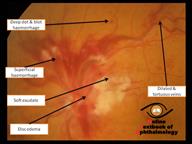
Acute CRVO (Figure-1) |
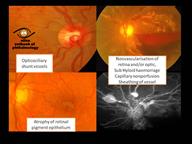
Chronic CRVO (Figure-2) |
|
Retinal Haemorrhages |
Cystoid macular edema Capillary nonperfusion Microvascular changes including microaneurysms and collateral vessels Subretinal fibrosis Optic disc venous-venous shunt/collateral vessels (opticociliary shunt vessels). |
Table 3: Enumerating various clinical presentation of CRVO.
Figure 1: Showing various clinical findings in acute CRVO (Click to enlarge the image)
Figure 2:Showing various clinical findings in chronic CRVO(Click to enlarge the image)
Criteria to Differentiate Ischemic from Non-Ischemic CRVO:[5, 6]
The first crucial step in the management of CRVO is to find out what type of CRVO an eye has because the prognosis, management and outcome of the two are totally different. Hayreh has enumerated tests to diagnose type of CRVO, which is divided into functional tests and morphological tests.
Function tests consist of visual acuity, peripheral visual fields, relative afferent pupillary defect, and electroretinography.
Morphological tests are ophthalmoscopy and fluorescein fundus angiography.
Tests in differentiating ischemic from non-ischemic CRVO during the acute phase, inorder of reliability:
1. Relative afferent pupillary defect (RAPD):RAPD is very reliable in uniocular CRVO, when the fellow eye is normal. (>0.9 Log unit; 80% sensitive, 97% specificity)
2. Electroretinogram (ERG): Next in order is ERG, which can be performed in all cases, even with bilateral CRVO or with only one eye. (b wave amplitude decrease <60%; 80% sensitive, 80% specificity)
Combined information from the relevant afferent pupillary defect and ERG, provides the most reliable way of differentiating the two types of CRVO - in as many as 97% of the cases.
3. Visual field (VF):Next in order of usefulness is the visual field (VF) plotting with a Goldmann perimeter, which is better than the visual acuity. (VF- defective V4e target; 92% sensitive, 80% specificity/ VA ≤20/400; 91% sensitive, 88% specificity)
4. Fundus Fluorescein Angiography (FFA)is usually much less useful than the functional tests during the acute stages of the disease. Typically the retinal capillary non-perfusion or obliteration is considered the diagnostic criterion of ischemic CRVO. Various studies have reported different criteria for defining ischemic CRVO versus nonischemic CRVO based on the extent of capillary nonperfusion (CNP) of the retina. The amount of retinal nonperfusion ranges from 10-30 disc areas. (Figure 3 & 4)
Multiple limitations
During the very early stages, in spite of retinal ischemia, retinal capillary non-perfusion may not be seen, because it takes time for the retinal capillaries to obliterate completely.
If there are extensive retinal hemorrhages, it is usually almost impossible to evaluate capillary non-perfusion accurately, because of the masking effect by the blood.
Ophthalmoscopyis the least reliable and the most misleading parameter and cannot be used as a sole discretion for differentiating the two groups.
Tabular Column enumerating the difference between Ischemic vs Non-Ischemic CRVO (Table- 3)
|
Non –Ischemic (Figure1) |
Ischemic |
|
|
Frequency |
75-80% |
20-25% |
|
VA |
Better than 20/200 |
Worse than 2/200 |
|
RAPD |
Slight /nil |
Marked |
|
Visual field defect |
Rare |
Common |
|
Fundus- |
Less retinal hemorrhage & cotton wool spots |
Extensive retinal hemorrhage & cotton wool spots |
|
FFA |
Good perfusion |
Non perfusion > 10 disc areas |
|
ERG |
Normal |
Reduced b-wave amplitude |
|
Prognosis |
50-60 % improve |
60% Rubeosis, NVG |
Table 4: Differentiating points in Ischemic Vs Non-ischemic CRVO
Figure 3 Showing FFA features of-Non ischemic CRVO (Click to enlarge the image)
Figure 4- Showing FFA features of – Ischemic CRVO(Click to enlarge the image)
Natural History of CRVO
Visual outcome [6]:
Natural History of Visual outcome in patients with Central Retinal Vein Occlusion of 667 consecutive patients by Hayreh and et al, showed that the visual outcome differs between the two types of CRVO, i.e., non-ischemic and ischemic - good in the former and poor in the latter. The visual outcome is also adversely influenced to some extent by several other factors, including increasing age, cerebrovascular disease, and diabetes mellitus, and non-ischemic CRVO by the development of foveal pigmentation and epiretinal membrane, and in ischemic CRVO by neovascular glaucoma.[6]
Ocular Neovascularization(NV) [7]:
Non-ischemic CRVO eyes do not develop NV unless there is an associated disease that can cause NV, e.g., diabetes mellitus or ocular ischemia.
The risk of developing anterior segment NV in ischemic CRVO exists mainly during the first 7-8 months of the disease. The maximum risk of developing NVG is about 45% in the 1st year. Current conventional wisdom is wrong in assuming that all eyes with iris or angle NV go on to develop NVG; 1/3 of eyes with iris NV and ¼ of eyes with iris and angle NV do not progress to develop NVG on follow-up. These facts of the natural history of ocular NV in ischemic CRVO are of great clinical importance in its management.[6-7] Cumulative chances of conversion of non-ischemic CRVO to ischemic CRVO during follow-up: This can occur within 6 months in 9.4% and reached almost its maximum within 18 months in 12.6%.
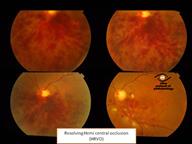
Resolution of retinopathy [6]:
In both types of CRVO, the retinopathy spontaneously resolves after a variable period. There is marked inter-individual variation in the time it takes to resolve - usually faster in younger than older people. Thus, both types of CRVOareself-limiting diseases, although during the period of activity they may produce various complications.
Complications of CRVO
CRVO is a sight-threatening disease. Visual loss may result from chronic macular edema and macular ischemia. Secondary complications (vitreous hemorrhage, retinal detachment, and/ or neovascular glaucoma) are due to retinal neovascularization.[8] The visual prognosis for patients with ischemic and non-ischemic CRVO differs. In non-ischemic CRVO 51% gained VA 20/40 or better without any treatment. The reduced baseline VA and extent of initial retinal ischemia correlated strongly with poor final VA.[9] Conversion of non-ischemic into ischemic CRVO has been observed in 10–33% of primary non-ischemic cases. Ischemic CRVO has a worse prognosis than the non-ischemic type; 73–93% of patients had a final VA of 20/200 or worse. [10]
NON-ISCHEMIC CRVO:
Long-term blinding complications are rare in this type. The major complication is chronic macular edema, leading to cystoid macular degeneration, and permanent central scotoma; however, the peripheral visual field always remains normal.
Other complications noted include:
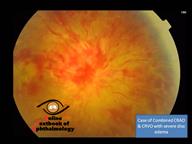
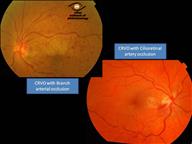
CRVO with Cilioretinal artery occlusion (CLRAO)/Central retinal artery occlusion/Branch retinal artery occlusion [11-16]:The pathomechanisms of CLRAO combined with CRVO are not well established. Two hypotheses have been proposed: (1) CLRAO occurs secondary to the raised capillary pressure caused by CRVO or (2) a primary reduction in perfusion pressure of the cilioretinal and retinal arteries, leads to decreased retinal circulation and subsequent venous stasis and thrombosis. Systemic blood pressure decrease and inflammatory or atherosclerotic retinal arterial disease have been. (Figure 5, Figure 6) Visual loss may be more profound, in eyes with concomitant cilioretinal artery occlusion (CLRAO) suggested as possible causes of reduced arterial perfusion pressure.
Figure 5: Showing Combined occlusion of CRAO & CRVO (Click to enlarge the image)
Figure 6: Showing CRVO with BRAO & Cilioretinal arterial occlusion(Click to enlarge the image)
CRVO with Non arteritic anterior ischemic optic neuropathy (NAION) [17-18]
The presence of thrombophilic abnormalities may contribute to the concomitant occlusion of posterior ciliary arteries and central retinal vein. Ischaemic optic neuropathy needs to be considered in patients with CRVO when the visual acuity is not consistent with the retinal pathology. Visual field defect as a predominant feature is in cases with concomitant Non arteritic anterior ischemic optic neuropathy (NAION) and CRVO.
ISCHEMIC CRVO:
The most important complication is the development of ocular neovascularization. Overall incidence is 45% among the ischemic CRVO eyes. Other complications of ischemic CRVO are vitreous hemorrhage, macular degeneration, optic atrophy, proliferative disease (traction retinal detachment /combined mechanics retinal detachment), phthisis bulbi or loss of eye.
Ocular Neovascularization (NV):
It is a complication of ischemic CRVO/HCRVO and major BRVO only. It may also manifest in other cases, only if associated diabetic retinopathy or other types of retinopathy with extensive retinal capillary obliteration or associated carotid artery disease is present.
Some noteworthy points to remember [19]:
- Every eye with ischemic CRVO does not develop ocular NV.
- When ocular NV develops, the commonest site is the anterior segment, much less frequently the posterior segment.
- The greatest risk of developing anterior segment NV is during the first 7 months, after which the risk falls dramatically to minimal.
- About 1/3 of the eyes with iris NV and about 1/4 of the eyes with both iris and angle NV never develop NVG. (Figure 7)
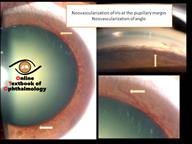
Figure 7: Showing NVI & NVA (Click to enlarge the image)
Papillophlebitis or Optic Disc Vasculitis [20]
Some mild CRVOs in patients younger than 50 years are classified as papillophlebitis or optic disc vasculitis - terms that suggest a benign course. Inflammatory optic neuritis or vasculitis is hypothesized as the cause. These eyes tend to have optic disc edema out of proportion to the retinal findings, cotton-wool spots that ring the optic disc, and occasionally cilioretinal artery obstructions or even partial central retinal artery obstructions. Although spontaneous improvement is common, the course is not always benign. Up to 30% of these patients may develop the ischemic type of occlusion, a final visual acuity of 20/200 (6/60) or worse occurs in nearly 40%, and neovascular glaucoma has been reported. (Figure 8)
Figure 8: Showing Papillophlebitis or Optic Disc Vasculitis. (Click to enlarge the image)
Differential Diagnosis [21-24]
As stated above, rarely is the full-blown picture of an ischemic CRVO confused with other disease entities (Table-4). However, nonischemic or long-standing CRVOs can appear similar to the retinopathy of carotid occlusive disease - the ocular ischemia syndrome.Both conditions are associated with blurred vision, and both may have transient visual loss. Blurring of vision when a darker room is entered after being in a brighter area is suggestive of carotid artery disease.[23] Although disc edema is always present in ischemic CRVO, may also be present in nonischemic CRVO, it is quite rare in carotid occlusive disease.
Although the veins are engorged in both diseases, they are generallynottortuous in the ocular ischemic syndrome. The retinal hemorrhages seen in carotid disease tend to localize to the midperiphery, instead of the posterior pole as seen in CRVO.
Hyperviscosity syndromes may produce bilateral retinopathy similar to CRVO and may, in fact, induce a true CRVO with thrombus formation. Simultaneous bilateral disease is an unusual finding in CRVOs but occurs more commonly in hypercoagulable and hyperviscous states. Diseases such as sickle cell disease, polycythemia vera, leukemia, and multiple myeloma are but a few of the possibilities. When a patient seeks treatment for bilateral CRVOs, especially simultaneous, the medical and laboratory evaluation should include a search for evidence of hyperviscous and hypercoagulable syndromes. Improvement in the affected eye is possible when a hyperviscosity syndrome is responsible and plasmapheresis is performed.[24] Severe anemia with thrombocytopenia can masquerade as a CRVO, and it is differentiated from a CRVO by a complete blood count with platelets. In addition, acute hypertensive retinopathy with disc edema may resemble bilateral CRVO.
|
Ocular ischemic syndrome |
Diabetic retinopathy |
Central retinal vein occlusion |
|
|
Age |
50s to 80s |
Variable |
50s to 80s |
|
Laterality |
80% unilateral |
Bilateral |
Usually unilateral |
|
Posterior segment signs |
|||
|
Retinal Vessels |
Dilated but not tortuous |
Dilated and beaded |
Dilated and tortuous |
|
Hemorrhage |
Dot and blot, mid-periphery, in deeper retina layers |
Dot, blot in deeper retina layers and flame-shaped in nerve fiber layer |
Flame-shaped in nerve fiber layer |
|
Micro aneurysms |
In midperiphery |
In posterior pole |
Variable |
|
Hard Exudates |
Absent |
Common |
Rare |
|
Optic Disc |
Normal |
Diabetic papillopathy (rarely) |
Swollen |
|
Retinal artery perfusion pressure |
Decreased |
Normal |
Normal |
|
Fluorescein angiography |
|||
|
Aretio-venous transit time |
Prolonged |
Usually normal |
Prolonged |
|
Choroidal filling |
Delayed, patchy |
Normal |
Normal |
|
Retinal vessel staining |
Arteries > veins |
Usually absent |
Veins > arteries |
Table -4: Table elaborating differentiating points of CRVO, Ocular ischemic syndrome (OIS), Diabetic retinopathy (DR).[21-22]
Management(Table- 5)
A general medical evaluation, to include medical history and physical examination with blood pressure evaluation has to be performed. Laboratory evaluation may include a complete blood count, glucose tolerance test, lipid profile, serum protein electrophoresis, chemistry profile, and syphilis serology. Additional testing, based upon the above findings, may be necessary. If a history of systemic clotting diathesis exists, further haematological tests such as lupus anticoagulant level, anticardiolipin antibody, and protein S and protein C levels should be considered. Elevated levels of homocysteine have also been associated with the development of retinal vascular occlusive disease.[25] Diagnosis and treatment of an associated disease is not expected to improve the visual outcome in the affected eye, but it may help to prevent subsequent obstruction in the fellow eye.
|
CENTRAL RETINAL VEIN OBSTRUCTION-Systemic & Ophthalmic workup: |
|
|
|
Table -5: Central retinal vein occlusion (CRVO) systemic & ophthalmic workup
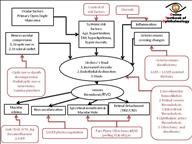
Therapeutic options for CRV(Flow Chart 1)
Mohamed et al [26] evaluated studies reporting on hemodilution, medical treatment with troxerutin and ticlopidine (inhibitors of platelet aggregation) and intravenous thrombolysis, and various surgical procedures to improve vision in CRVO. None of the management could provide reproducible results and the procedures also carry the potential for serious adverse effects such as stroke.
The reviews by Squizzato et al [27] and Lazo-Langner et al [28] suggest that antithrombotic therapy, with low molecular weight heparin (LMWH) showed limited potential in management of the CRVO.
Following a vitrectomy approach, several surgical procedures including internal limiting membrane peel, radial optic neurotomy and direct retinal vein cannulation with injection of fibrinolytics, have all been advocated for the management of macular edema in CRVO. However the mechanism of action of these interventions remains contentious and their safety and efficacy have not been evaluated.[29-33]
McAllister et al & Browning DJ et al had reported the technique which utilized a high power (argon or Nd: YAG) laser spot to rupture Bruch’s membrane and a second spot to rupture a major branch of the retinal vein next to the first laser spot. Although the technique is relatively noninvasive and readily accessible it has high potential.[34-35]
Flow Chart-1: Showing the pathogenesis & the options available for the management of the same at the particular pathogenic stage of VO. (Click to enlarge the image)
Current Management of CRVO(Figure-9-13)
Treatment for patients with retinal vein occlusion (RVO) is directed at:
Eliminating macular edema (MO) to improve vision, prevention/ treatment of retinal neovascularization, and anterior segment neovascularization and neovascular glaucoma.
Treatment also involves management of predisposing risk factors, such as diabetes and hypertension.
Macular oedema
Laser photocoagulation[36-38]:
There is a very limited role for grid photocoagulation to treat the macular edema that develops after CRVO. TheCentral Vein Occlusion Study Group (CVOS)showed that while macular edema was reduced, there was no improvement in visual acuity after grid treatment and no difference in final visual outcome compared to control eyes. Focal laser photocoagulation in those few cases with visible leaking vascular malformations / aneurysms in the macula causing macular edema can be attempted as an attempt at macular edema regression.
Intravitreal steroids
IVTA[39] :
The rationale for the use of intravitreal triamcinolone acetonide (IVTA) to treat macular edema is that corticosteroids reduce retinal capillary permeability and inhibit the expression of the VEGF gene and the metabolic pathway of VEGF.
TheSCORE-CVOtrial showed that patients treated with triamcinolone 1 mg had equal gains in visual acuity but fewer steroid-related side effects than those treated with 4 mg of the drug, and both groups had better visual acuity than patients who were in the observation group.
Availability of newer and safer pharmocological agents has led to the disuse of IVTA as a first line therapy to treat macular edema in CRVO.
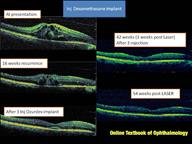
Dexamethasone Implant[40-41]
Dexamethasone, in its free form, has a short half-life, which limits its clinical usefulness in its naïve form. This was circumvented by using a biodegradable pre-filled applicator which has the property for sustained release. This implant containing 0.7mg of dexamethasone (Ozurdex, Allergan) was analysed in theGENEVA studyprogramme.[40]
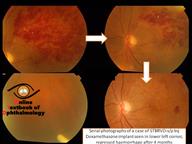
The mechanism of action of dexamethasone is similar to that of triamcinolone but is a more potent corticosteroid. The implant offers sustained and controlled release of the drug to minimise the potential side effects of intra-ocular steroids. Geneva trial showed that the percentage of eyes with ≥ 15 letter gain in BCVA was significantly higher in both implant (0.35 mg/ 0.7 mg) groups compared with sham at days 30 to 90 with a peak effect at 60 days. Subgroup analyses of the BRVO and CRVO subjects showed a significantly greater number achieved ≥ 15 letter gain from 30 to 90 days than sham treated eyes.
In terms of safety, raised IOP peaked at month two (3.2% of patients had an IOP>35 mmHg), but declined significantly by month three and was close to 0% by month six, with 19% of patients requiring an IOP-lowering agent at month six and 0.7% of patients requiring any IOP-lowering surgical procedures. Similarly, rates of cataract progression were low with 7% progression at month six, compared to 4% in the sham group. The results further indicate that eyes treated earlier had a better chance of visual acuity gain, and that those treated later (i.e. controls that were subsequently treated) never achieved the final visual acuity gains of those treated promptly.
SHASTA studyhas demonstrated that treatment with 2 or more DEX implants, alone or with other adjunctive RVO treatment, improves visual acuity, reduces central retinal thickness, and has an acceptable safety profile in patients with newly diagnosed and previously untreated RVO-associated macular edema.[41]
Anti-VEGF Therapies:
Anti-VEGF agents are now a popular choice for treatment of MO due to CRVO based on the fact that VEGF-A is a key cytokine that mediates vascular leakage and causes MO in RVO.
Ranibizumab[42-46] (0.5mg/0.05ml)
Ranibizumab is a humanized recombinant monoclonal antibody fragment that selectively binds to human VEGF-A, and prevents it from binding to its receptors. The interval between two injections is at least 4 weeks. The pivotal Phase III randomized controlled trial that evaluated ranibizumab (0.3mg and 0.5mg) in MO due to CRVO was theCRUISE study.[42] The results showed a significant anatomical and visual improvement in both treatment groups 7 days after the intravitreal injection. PRN treatment with monthly follow-up maintained the visual improvements achieved after the first 6 months of treatment. Patients in the control group who received PRN treatment after the first 6 months showed an anatomical improvement similar to that in the treatment groups but less visual improvement.
Patients who completed the 12 month CRUISE trial entered an open-label, single arm, multicentre follow-up study called theHORIZON extension studyin which they could continue to receive 0.5mg ranibizumab on a PRN basis. Key finding from the HORIZON was that long-term use of ranibizumab was well-tolerated. MO not treated in the second year was also associated with worse visual and anatomical outcomes. There are clear differences in outcomes for BRVO and CRVO patients. CRVO patients required frequent follow-up and continued ranibizumab therapy to control oedema.[43]
TheRETAIN Studyincluded patients with CRVO and BRVO in a prospective follow-up of a subset of patients from two phase three trials of ranibizumab in RVO. The mean follow-up was 49.7 months for CRVO patients, where 14 of 32 patients (44%) had edema resolution, with 71% receiving their last injection within two years of treatment initiation. However, in unresolved patients, a mean number of 5.9 injections of ranibizumab were given in year 4. In eyes with resolved disease had greater improvement in BCVA compared to baseline (25.2 vs. 4.3 letters; p= 0.002).[44]
TheCRYSTAL study, ongoing long-term trials support the safety and efficacy of intravitreal ranibizumab for treatment of CRVO with dosing on an as-needed basis after stabilization of disease.[45]
Enrolled patients with CRVO for treatment with 0.5 mg ranibizumab, received monthly injections until visual acuity was stable for 3 consecutive months, and were followed out to 12 months thereafter with treatment on an as-needed, or PRN, basis. The CRYSTAL study also enrolled patients with more advanced disease than studied in previous clinical trials for CRVO involving ranibizumab. The mean change in BCVA at month 12 was 12.3 letters after a mean 8.1 injections.
TheCOMRADE-Cwas the first study to compare the efficacy and safety of ranibizumab 0.5 mg with intravitreal dexamethasone implant 0.7 mg (Ozurdex, Allergan) therapy, for treatment of visual impairment due to macular edema secondary to CRVO. Ranibizumab was administered PRN until the study eye was stable. The dexamethasone implant 0.7 mg was administered once at baseline and then sham implant injections were made PRN. Patients were monitored for 6 months.[46]
Insignificant change in IOP was seen in the ranibizumab group compared with a brief rise in IOP that returned to baseline by month 6 in the dexamethasone implant group. COMRADE-C demonstrated an impressive visual acuity gain among patients treated with ranibizumab for CRVO compared to dexamethasone group.
Aflibercept[47-49]
The pan-VEGF-A, VEGF-B and placental growth factor (PlGF) blocker, aflibercept, continues to be evaluated in clinical trials and has shown promise in the treatment of MO associated with vein occlusions.COPERNICUSwas a phase three, prospective, randomized, double-masked trial (n=187) comparing monthly intravitreal injection of aflibercept 2mg (n=115) with sham (n=74) for the treatment of MO secondary to CRVO.[47]
This study also showed that unless treatment is instigated early, there is likely to be a great degree of irrecoverable visual loss. In summary, therefore, although the anatomical response (drying up of the macula) in the sham/aflibercept PRN patients largely caught up with that regularly treated aflibercept group, the BCVA did not. This may suggest that persistence of structural change can lead to irreversible functional loss.
Progression to ocular neovascularization during the first 52 weeks was eliminated in the aflibercept group (0% vs. 6.8% in the sham treatment group P=0.006). All neovascularization seen in the sham group occurred in the anterior segment. The results also suggest that once disease control was obtained over several months of loading, less frequent injections were needed subsequently.
GALILEOwas a phase 3, randomised, double-masked trial comparing intravitreal aflibercept with sham for MO secondary to CRVO. There was no crossover in this study. The visual and anatomic improvements seen after fixed, monthly dosing at week 24 were largely maintained when treatment intervals were extended. Patients with macular edema following CRVO benefited from early treatment with intravitrealaflibercept.[48]
NEWTON study. iIs a phase 4, prospective, single arm, single-centre, interventional study testing whether the interval between injections in eyes with macular edema secondary to central retinal vein occlusion (CRVO) previously treated with bevacizumab (Avastin, Genentech) or ranibizumab (Lucentis, Genentech) increased when switched to aflibercept.
Patients enrolled were previously treated with ranibizumab or bevacizumab for 6 months and had an occurrence of macular edema when extended beyond 4-week dosing intervals. Patients received 2.0 mg aflibercept on a treat-and-extend regimen. The macular edema free period increased from an average of 39 days to 62 days.[49]
Bevacizumab[50-51]
Currently, increasing short-term data support the fact that multiple intravitreal bevacizumab injections reduce MO due to CRVO.[50-51] The most common treatment regimen is two to three injections over the first five to six months. However, further randomized, controlled trials are required to assess long-term safety and efficacy of intravitreal bevacizumab.
So Which Anti-VEGF to choose??
ACochrane meta-analysison anti-VEGF agents for the treatment of MO secondary to CRVO included high-quality data from 937 participants in six RCTs, who were either treated with intravitreal anti-VEGF (aflibercept, bevacizumab, ranibizumab or pegaptanib sodium) or sham injection.[52] It found that participants receiving anti-VEGF therapy were 2.71 (95% confidence interval for risk ratio 2.10 to 3.49) times more likely to gain at least 15 letters of visual acuity at six months compared to participants treated with sham. High-quality evidence from five trials suggested anti-VEGF treatment was associated with an 80% lower risk of losing at least 15 letters of visual acuity at six months compared to sham injection (RR 0.20; 95% CI 0.12 to 0.34). In addition, high-quality evidence from six trials suggested that anti-VEGF treatment was associated with an 82% lower risk of developing iris neovascularization at six months compared to sham injection (RR 0.18; 95% CI 0.09 to 0.36).
Treatment Algorithm for CRVO
A. Treatment of risk factors (to be managed by patient’s physician).
B. Ophthalmic management
I. NON-ISCHAEMIC CRVO
Baseline
Visual acuity measurement, colour fundus photographs and fluorescein angiography, OCT, IOP, gonioscopy if ischaemic CRVO is suspected.
If no iris or angle NV and there is OCT evidence of MO:
If visual acuity is 6/96 (20/320) or better, commence on either intravitreal anti-VEGF therapy or Ozurdex implant
If visual acuity is less than 6/96 (20/320), the potential for significant improvement in visual acuity is minimal and the risk of ocular neovascularisation is high.
However, eyes with VA< 6/96 (20/320) may be offered treatment as some of these eyes may respond. The patients should be watched for NVI/NVA
If visual acuity is better than 6/12 (20/40), it is reasonable to observe the patient for spontaneous resolution as per the judgment of the treating ophthalmologist.
Choice of agent
Ranibizumab / Bevacizumab/ aflibercept are the anti-VEGF agents recommended by most of the studies for treatment of MO due to CRVO. Dexamethasone implant (Ozurdex) can also be used for this condition. There is no visual acuity or central macular thickness restriction in the commencement of treatment with any of these agents.
Although any of these drugs may be used as first line for this condition, anti-VEGF is preferred in eyes with history of glaucoma (diagnosed / suspected) and younger patients who have clear crystalline lens. Dexamethasone implant (Ozurdex) is a better choice in patients with recent cardiovascular events and in those who do not favour monthly injections.
Re-treatment
At each follow-up visit, visual acuity, macular thickness and IOP should be assessed and the presence of NVI/NVA assessed.
If Anti-VEGF is the first line of treatment,
Monthly intravitreal injections are continued until maximum visual acuity is achieved, which is defined as stable visual acuity for three consecutive monthly assessments while on therapy. (CRUISE trial[42])
If no improvement in visual acuity over the course of the first three injections is observed, cessation of treatment or use of alternate group of drugs may be considered. Alternately, injections on a PRN basis from initiation have also been employed in managing RVO associated macular edema.
If Dexamethasone implant is the first line of treatment, re-treatment may be required at four to six monthly intervals until visual stability is obtained. A few of the patient may require more frequent dosing (i.e. less than 16 weeks interval). However, more frequent and repeated treatments with Ozurdex increase the risk of adverse events and these should be discussed with the patient. Patients should be monitored for raised intraocular pressure (IOP) and formation or progression of cataract.
After 3 to 6 months of management with either of the intravitreal drugs mentioned above FFA can be performed to identify CNP areas or focal leakages around the macula, supplemental scatter LASER photocoagulation / focal LASER can be done to prong the effect of the intravitreal injections.
Switching agents
If an anti-VEGF agent is stopped due to lack of efficacy, there are no randomised controlled trials that provide evidence that switching to another anti-VEGF agent may be effective. However, given our experience with switching anti-VEGF agents in neovascular age related macular degeneration, it may be worthwhile switching to another anti-VEGF agent and further monthly injections for three months may be given to assess the efficacy of the switch.
There is a good rationale to switch from dexamethasone implant to an anti-VEGF agent and vice versa as the different mode of actions of these agents may aid in resolution of MO. However, the long term outcomes of sequential or combination treatment of anti-VEGF agents and steroids remain unclear.
II. ISCHAEMIC CRVO
If iris or angle neovascularisation occurs and the anterior chamber angle is open:
After decongesting the eye with intra vitreal ± intra cameral anti VEGF early panretinal photocoagulation (PRP) is recommended with review at two weeks initially and then less frequently as regression occurs.
If iris or angle NV is present with a closed angle and raised intraocular pressure :
In an eye with good visual potential urgent PRP is recommended with cyclodiode laser therapy / tube shunt surgery. The latter is preferable if the angle closure is established. If the intraocular pressure is normal or normalizes with the above therapy, intravitreal anti-VEGF agent can be considered. If the intraocular pressure is significantly elevated it should be managed as above with topical and medical management in addition.
In an eye with potentially good visual prognosis and associated with poor visualization of the fundus due to cataract and /or vitreous haemorrhage, cataract surgery with pars plana vitrectomy with endo-photocoagulation / endo-cyclophotocoagulation ± intra vitreal anti VEGF can be planned.
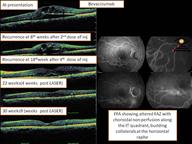
Figure 9: Serial Oct of CRVO managed with Inj Ranibizumab with supplemental modified grid LASER (Click to enlarge the image)
Figure- 10 Serial OCT of a Case of CRVO managed with Inj Bevacizumab (Click to enlarge the image)
Figure 11- Image showing regression of ischemic CRVO post multiple Injection Anti VEGF (Click to enlarge the image)
Figure-12- Serial OCT of a case managed with Inj Dexamethasone implant showing multiple recurrences. (Click to enlarge the image)
Figure-13 Serial OCT of a CRVO case managed with Inj Dexamethasone implant and LASER (Click to enlarge the image)
Hemi retinal Vein Occlusion (HRVO)
Pathogenesis of Hemi retinal Vein Occlusion (HRVO)[1,2]
The pathogenesis of this type of RVO is similar to that of CRVO. Usually only one of the two trunks of the CRV is involved. 20% of eyes bifurcation of the trunk occurs posterior to the lamina cribrosa (Figure-14 ). Occasionally, however, both trunks may be involved - presumably due to site of occlusion being in the main trunk of CRV after the union of the two trunks, and this on routine examination would appear to be ordinary CRVO.
Figure 14- Showing the drainage of the two branches (superior & inferior) of central retinal vein which join beyond the lamina cribrosa, showing the pathogenesis /site of thrombosis in HRVO.(Click to enlarge the image)
Demographic characteristics[1, 2]
More so the demographic features of the HCRVO are similar to CRVO except the following.Recurrence of RVO in the same and/or fellow eye-Non-ischemic HCRVO being 3.5% within 2.2 years, for ischemic HCRVO being 7.4% at 0.4 year.
Risk of recurrence of same type of RVO in the same eye-For non-ischemic HCRVO it is 3.7% within 6.1 years. No recurrence was seen in ischemic.
Clinical futures(Figure-15)
The signs and symptoms are more so the same as CRVO except hemorrhages involving the whole hemisphere of the fundus. Often erroneously diagnosed as a major BRVO.
The symptomatology in non-ischemic HCRVO is usually similar to that described for nonischemic CRVO above.
In ischemic HCRVO the visual loss is much worse, involving the visual field in the sector of the retina involved as well as central visual loss from macular involvement.
Figure- 15- Showing a case of HRVO showing resolution after management with Anti VEGF.(Click to enlarge the image)
Differentiation of hemi-CRVO from major BRVO[53]: (Table- 6)
This distinction is important because major BRVO is almost always of ischemic type while HCRVO may be non-ischemic (in 78%) or ischemic (22%) type; with very different prognosis and complications
|
BRVO |
HCRVO |
|
|
Site of occlusion |
Arteriovenous crossing, rarely at the disc |
Optic disc |
|
Corresponding part of the optic disc |
Normal |
Edema |
|
Location of venous collaterals |
On the retina away from the optic disc |
either on the optic disc or within the optic nerve |
|
Quadrants involvement |
One , rarely multiple sits of BRVO |
Two quadrant , nasal always involved |
|
Incidence of glaucoma |
Less |
High |
Table 6: Differentiating points of BRVO from HCRVO.
In differentiation of non-ischemic from ischemic HCRVO, the various tests discussed above in CRVO do not help much except that the visual fields with a Goldmann perimeter show, in addition to central scotoma, a dense segmental defect with larger isopters, and fluorescein angiography later on shows retinal capillary non-perfusion in the involved retina.
Neovascularization in ischemic HCRVO is very different from that seen with ischemic CRVO 58.1% present with NV overall, with retinal NV in 41.9% and disc NV in 29% and anterior segment , iris NV in 12.9%, angle NV in 6.5%. The severer and more extensive the retinopathy, the more marked the NV. [53]
The management of the HCRVO is same as discussed above for CRVO. (Figure16)
Figure 16- Serial OCT showing case of HRVO managed with Inj Dexamethasone showing recurrence. (Click to enlarge the image)
Branch retinal vein occlusion BRVO
Pathogenesis of Branch retinal vein occlusion
Arteriosclerosis and arterio-venous crossing of retinal branch vessels play important roles in development of BRVO. At the site of occlusion in BRVO, the retinal arteriole lies anterior to the occluded vein in 93%-100% of cases.[54]
BRVO is seen more commonly in the temporal than nasal part of the retina, and of the temporal retina more frequently in the superior than inferior quadrant. The arterio-venous crossings have been shown to be more frequent in the supero-temporal quadrant than elsewhereand situated closer to the optic disc in the supero-temporal than infero-temporal quadrant.[55]
In addition to above all, focal phlebitis is a well known cause of BRVO, e.g., in toxoplasmic chorio-retinitis and retinal vasculitis. Similarly BRVO is seen in dysproteinemias, sickle cell disease and other hematologic disorders wherein the hypercoagulability or hyperviscosity results in RVO. Unlike CRVO and HCRVO, glaucoma and raised IOP play no role in the pathogenesis of BRVO.[56]
Demography[1, 2]
More so the demographic features of the BRVO is discussed with CRVO as above except the following-
Risk of same type of RVO developing in the fellow eye:
Within 2 years the fellow eye developed major BRVO in 3.4%, and within 4 years in 6.6%. For macular BRVO it is 4.0% at 3.3 years.
Clinical features
Major BRVO (Figure-17) is invariably symptomatic, with visual blurring involving usually the central vision and also frequently the sector of visual field corresponding to the area of the retina involved. In macular BRVO there is always the central visual disturbance, with normal peripheral vision. Since macular BRVO (Figure 18) always involves a sector of the macular retina radiating centrifugally from the fovea, there is no difficulty in differentiating it from major BRVO. Differential diagnosis of BRVO are mentioned in the following table (Table No- 7)
Figure-17-Showing a case of Supero-temporal BRVO managed with Inj Dexamethasone implant.(Click to enlarge the image)
Figure 18- Macular BRVO managed with Inj Ranibizumab.(Click to enlarge the image)
| DIFFERENTIAL DIAGNOSIS OF BRANCH RETINAL VEIN OBSTRUCTION | ||||||
|
Table 7: Differential diagnosis of branch retinal vein occlusion
Complications of BRVO
In general, BRVO has a good prognosis; 50–60% of eyes have been reported to have a final visual acuity (VA) of 20/40 or better even without any treatment.[57]
Macular changes
A poor visual prognosis has been reported in patients with chronic macular edema or macular ischemia. Generally, it is difficult to determine visual prognosis for patients with BRVO in the acute phase of the disease. Chronic ME has a poor prognosis in terms of final VA only 14% of eyes with chronic ME retained a VA of 20/40 or better, while 86% had a final VA of 20/50 or worse. [58] (Figure 19) Worse visual prognosis in cases of ischemic ME compared to perfused ME. [59] VA is a very sensitive indicator of the oxygen situation in the macula. For this reason, pre-treatment VA may be an important prognostic factor.
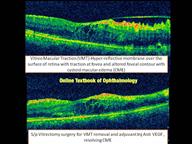
CME associated with pull mechanism, like VMT/ERM which are responsible for non responding CME may require vitrectomy surgery along with adjuvant intra vitreal Anti VEGF/Steroid. (Figure 20)
Figure- 19- Showing FFA of a case of BRVO showing macular ischemia, NVE , CNP areas collaterals at the edge of normal and ischemic retina. (Click to enlarge the image)
Figure- 20: Showing OCT images of a case status post vitrectomy for Vitreo macular traction (VMT) removal for persistent CME (Click to enlarge the image)
Neovascularization & its sequel(Figure- 21)
NV is seen much less commonly, 28.8% can develop NV overall, with retinal NV 24.1% and optic disc NV 28.8% and anterior segment NV extremely rare (iris NV in 1.6% and angle NV in 0.5%)- the latter is seen essentially in eyes with BRVO involving half or more of the retina.
Vitreous hemorrhage from retinal/disc NV usually occurs during the late stages of the disease. Sometimes the vitreous hemorrhage can occur from intraretinal microvascular abnormalities secondary to RVO or development of posterior vitreous detachment. Therefore,it is important to be aware of the fact thatpresence of vitreous hemorrhages in RVO does not always mean the presence of retinal/disc NV. [1, 7]
Figure 21- Showing NVE secondary to BRVO managed with sectoral PHC (Click to enlarge the image)
Retinal detachment(Figure 22)
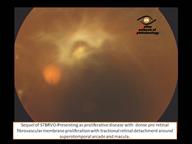
Retinal Detachment with BRVO-Tractional retinal detachment TRD occurs due to fibro-vascular proliferation and incomplete posterior vitreous detachment. Long standing TRD can case eitherretinoschisis or combined mechanism retinal detachment (CRD). The pathogenesis of such detachment is unclear though it is postulated that the ischemic retina becomes atrophic so has increased risk of retinal tear formation.[60]
Figure 22- Showing fibro vascular proliferation over supero-temporal arcade with TRD secondary to STBRO. (Click to enlarge the image)
Management of BRVO:
The management is the same as CRVO but with better visual prognosis and minimal interventions.
Medical & Ophthalmic workup
- Complete history & physical examination
- Complete Ophthalmic examination
- Fundus fluorescein angiography
- Blood pressure
Systemic association with BRVO
- Resistance to activated protein C (especially factor V Leiden mutation)
- Protein C or protein S deficiency
- Deficiency of antithrombin III
- Genetic mutation in the prothrombin (factor II) gene
- Anti-phospholipid antibodies
- Hyperhomocysteinemia
Treatment
Current treatment options focus on the sequel of the occluded venous branch, such as ME, retinal neovascularization, vitreous hemorrhage, and traction retinal detachment. There have been a number of treatment modalities advocated for the management of BRVO
Medical management for BRVO[61-65]
Anti –aggregative therapy & fibrinolysis. There is no general current acceptance of this treatment.
Isovolemic hemodilution. The use of hemodilution to treat BRVO is currently not accepted. Sheathotomy & vitrectomy. To date no randomized clinical trials on the surgical treatment of BRVO have been published. Any evidence supporting these procedures is based on non-randomized case series only.
Treatment of BRVO and macular oedema
Observation
The visual outcome following the natural course of BRVO is well documented.[57]In general, BRVO has a good prognosis: 50–60% of eyes have been reported to have a final VA of 20/40 or better even without any treatment.[57]The natural course of BRVO is determined by the site and degree of occlusion, the integrity of arterial perfusion to the affected sector, and the efficiency of the developing collateral circulation. A worse visual prognosis in cases of ischemic ME compared to perfused ME.
Although visual improvement is more common in BRVO than CRVO, few studies reported improvement beyond 6/12.[66] The Branch Vein Occlusion Study (BVOS) was a multicentre, prospective, randomized trial designed to study the natural history and effect of laser treatment in this condition. This study demonstrated that, after three years of follow-up and based on available data on 43 participants, 28 (63%) of laser-treated eyes had improved ≥2 lines of vision, compared with 13 (37%) out of 35 untreated eyes that remained in the study for 36 months.[67]
Laser photocoagulation[67]
The BVOS study reported that 40% of eyes (n=43) undergoing macular laser had worse than 20/40 visual acuity at three years, and 12% of treated eyes had 20/200 or worse visual acuity at three years.[67]
Laser photocoagulation in isolation is seldom performed in the current scenario, wherein the eyes are treated primarily with an intravitreal anti-VEGF or steroid. Laser as a rescue therapy in non-responding eyes or as an adjunct to injections to decrease the burden of injections is what is recommended. Laser photocoagulation using a 50 to 100um spots size is used to treat BRVO related MO, faint grey discoloration of the retina is the expected endpoint , the power setting required will vary from patient to patient and should be adjusted accordingly. An average of between 20 to 100 applications (depending on the area of vascular leakage) are required in a grid pattern to the areas of vascular leakage but avoiding the foveal avascular zone and any surrounding areas of capillary closure. Collaterals should be avoided.
Intravitreal steroids
Intravitreal triamcinolone acetonide (IVTA)[68]
The long-term safety and efficacy of IVTA (using preservative-free triamcinolone) was evaluated in theStandard Care Versus Corticosteroid for Retinal Vein Occlusion Study(SCORE) that showed that this treatment is not beneficial for this condition laser was more efficacious than IVTA in treatment of MO associated with BRVO. TheSCORE-BRVO trialshowed similar results as the SCORE-CRVO trial with both groups (4 mg and 1mg) had better visual acuity than patients who were in the observation group.[68]
Dexamethasone[40]
TheGENEVA studythat evaluated safety and efficacy of an intravitreal implant of dexamethasone (Ozurdex; Allergan Inc., Irvine, California, USA) in participants with MO secondary to retinal vein occlusion showed that the outcome of this drug in MO due to BRVO was better than in the control participants. In the GENEVA study programme.
In terms of safety, raised IOP peaked at month two (3.2% of patients had an IOP>35 mmHg), but declined significantly by month three. Nineteen percent of patients required an IOP lowering agent at month six and 0.7% of patients required IOP lowering surgical procedures. Cataract incidence and progression is a significant complication of Ozurdex therapy.[40]
Intravitreal anti-VEGF therapy
Ranibizumab(Lucentis, Novartis) [69-72]
TheBRVOtrial, it is a randomized multicenter study in patients with macular edema secondary to branch retinal vein occlusion.
At six months, the mean gain in VA was +16.6 and +18.3 letters (0.3 and 0.5 mg respectively). From months three to five, a single application of rescue laser photocoagulation was also allowed in all study arms if hemorrhages had cleared sufficiently to allow safe application of laser and the following criteria were met: Snellen’s equivalent BCVA ≤20/40 or mean central subfield thickness 250µ.[69]
Following the first six months, all patients were enrolled into an open-label extension for an additional six months and the overall 12 months’ results suggest that the visual gain established in the first six months can be retained with a slightly less intensive pro re nata (PRN) therapy with ranibizumab (an average of 5.7 injections in the first 6 months, vs. 2.7 injections in the second PRN six month phase.[70]
Further to BRVO the open label extension of theHORIZON triallooked at 304 previous BRAVO patients with MO secondary to BRVO to assess the long term safety and efficacy of ranibizumab treatment. There were no new adverse events identified. As such the long term administration of ranibizumab in PRN regimen was well tolerated and efficacious in patients with MO secondary to BRVO. [43]
The more recentRETAIN Studyincluded 34 patients with BRVO in a prospective follow-up of a subset of patients from two phase three trials of ranibizumab in RVO. It shows that the long-term outcomes of BRVO eyes treated with ranibizumab was excellent, although about half of them required continuing treatment.[44]
TheBRIGHTER studyis an ongoing long-term trials support the safety and efficacy of intravitreal ranibizumab for treatment of BRVO with dosing on an as-needed basis after stabilization of disease, patients randomized 2:2:1 to receive 0.5 mg ranibizumab (group 1), 0.5 ranibizumab plus laser (group 2), or laser alone (group 3) for treatment of BRVO. Patients received monthly injections until visual acuity was stable for 3 consecutive months, and were followed out to 12 months thereafter with treatment on an as-needed, or PRN, basis. The confirmed the efficacy of ranibizumab for BRVO with no additional benefit of laser. There were mean gains of BCVA from baseline of 14.4 letters in group 1, 14.8 letters in group 2, and 6.0 letters in group 3 (P < .0001). Patients received a mean 4.8 injections in group 1 and 4.5 in group 2. There was no difference in visual acuity outcomes among patients who had ischemic versus nonischemic BRVO. These likely represent patients who would not have been studied in pivotal clinical trials.[71]
TheCOMRADE-B STUDYis the first head-to-head trial comparing ranibizumab injections with a 0.7-mg dexamethasone retinal implant (Ozurdex, Allergan).This study also involved patients with a long duration of disease, which differs from previous studies. Ranibizumab patients received 3 initial doses, followed by PRN injections until month 6 of treatment, and the dexamethasone patients received initial injection of the dexamethasone implant followed by sham injections. The study showed that ranibizumab 0.5 mg was significantly more efficacious than the implant over 6 months for treatment of BRVO. The ocular pharmacological activity of the steroid implant waned after 3 months.[72]
Aflibercept(Eylea, Bayer) [73]
Based on the VIBRANT Study.[73] A total of 183 subjects with treatment naïve MO due to BRVO with sufficient clearing of macular haemorrhage to allow laser treatment at baseline and best corrected visual acuity of 24 – 73 ETDRS letters were randomized to four weekly aflibercept versus macular laser. After 6 monthly IAI, injections every 8 weeks maintained control of macular edema and visual benefits through week 52. In the laser group, rescue IAI given from week 24 onward resulted in substantial visual improvements at week52 arm. The functional outcomes mirrored the significantly more reduction in mean central retinal thickness in the aflibercept arm (-280.5μm) compared to the laser arm (-128.8μm).
Bevacizumab[74-75]
Currently, increasing short-term data support the fact that multiple intravitreal bevacizumab injections reduce MO secondary to BRVO including those that had failed previous laser treatment. The most common treatment regimen is two to three injections over the first five to six months.
Evidence-based management of BRVO in clinical practice:(Figure-23-25)
The natural history of MO due to BRVO indicates that MO may resolve or reduce over time with an approximate mean gain of 7.3 ETDRS letters at six months (BRAVO sham arm). However, a delay of six months in initiating anti-VEGF therapy in this condition also results in an inferior visual outcome compared to prompt treatment at diagnosis.
The macular laser has been the treatment of choice for this condition for the last 20 years. However, with the availability of anti-VEGF agents, the role of the laser as first-line treatment should be restricted to patients unsuitable or unwilling to receive anti-VEGF therapy.
Anti-VEGF agents (ranibizumab and aflibercept) have shown significant visual gains in patients with MO due to BRVO. The BRAVO trial followed by the HORIZON and RETAIN showed that ranibizumab with rescue laser is superior to sham. The studies also showed that if PRN treatment is commenced after maximal visual acuity gain, patients need to be monitored monthly initially followed by at least three monthly to sustain the visual benefit. TheVIBRANT trialshowed that four weekly aflibercept is superior to macular laser at six months.
As inflammation likely plays a role in MO due to RVO. Ozurdex was the first intravitreal agent that was recommended by the GENEVA study. More frequent dosing every 3-4 months (than six-monthly used in GENEVA) is required to produce optimal results. The impact of frequent dosing is the higher rate of progression of cataract.
Treatment of neovascularisation
It is recommended that sector laser photocoagulation is applied once retinal or optic disc neovascularization occur. Fluorescein angiography is not usually necessary prior to laser because the area of ischemia is visible clinically.
Treatment algorithm for BRVO
A. Treatment of risk factors by patient’s physician.
B. Ophthalmic management of BRVO
I. NON-ISCHAEMIC BRVO
Baseline
1. If VA better than 6/12, it is reasonable to regularly observe progress for three months.[57]
2. If VA is 6/12 or worse with macular oedema and haemorrhages are not masking fovea:
a) FFA is recommended to assess foveal integrity
b) If no macular ischemia is identified, regularly observe for three months if macular oedema is mild and in opinion of clinician likely to spontaneously improve (30% chance)
c) If mild to moderate macular ischemia is present consider treatment with ranibizumab or Ozurdex if spontaneous improvement is unlikely
d) If severe macular ischemia is present — no treatment is recommended, and regularly observe for NV formation
3. If VA 6/12 or worse + macular oedema and haemorrhages are masking macula
a) Monthly ranibizumab or baseline Ozurdex for three months.
b) Perform FFA at 3 months to assess foveal integrity
c) If severe macular ischemia is found to be present at three months, no treatment will likely be beneficial and further therapy should be carefully considered
At three months follow-up
1. Consider modified grid laser photocoagulation if persistent macular oedema, no or minimal macular ischemia and other treatments unsuccessful or unavailable.
2. If VA >6/9 or no macular oedema detected, continue to observe if initially observed. If on anti-VEGF or Ozurdex therapy, continue as suggested in MO due to CRVO.
Further Follow-up
1. If under observation only, follow-up three monthly intervals for 18 months
2. In case of recurrence or new macular oedema, consider re-initiating intravitreal ranibizumab or Ozurdex therapy
ISCHAEMIC BRVO
a) Watch carefully for NV
b) If NVE — consider sector laser photocoagulation applied to all ischaemic quadrants. Intravitreal anti-VEGF may also be given in combination with laser.
c) Follow-up at three monthly intervals for up to 24 months.
Figure 23- Serial OCT showing management of macular BRVO with dexamethasone implant (Click to enlarge the image)
Figure24- Showing BRVO s/p multiple dosages of Bevacizumab, FFA showing CNP areas treated with laser for recurrent ME. (Click to enlarge the image)
Figure- 25 Case of BRVO with serial OCT, s/p multiple dosage Ranibizumab 5 months later treated with grid PHC to the leaky micro-aneurysms.(Click to enlarge the image)
Unanswered questions:
The role of anti VEGF in treatment of patients with visual acuities better than 20/40 was not addressed by these studies. This is a significant issue given that, in the natural history arm of CVOS, 29% of subjects presented with a visual acuity ≥20/40.
The efficacy of ranibizumab in the treatment of patients with severely reduced visual acuity and, potentially, advanced macular ischemia, was not evaluated. The presence of an afferent pupillary defect was an exclusion criterion for both CRUISE and BRAVO, thus eliminating many subjects with ischemic CRVO. VEGF has also been shown to have neuroprotective properties; such qualities may acquire increased significance in the context of significant capillary nonperfusion.
Because patients with RVO are in general younger than patients with AMD and more likely to be involved in the working world, it is often important that they recover their vision quickly so that they can drive to work and function in the workplace. The point of risk-benefit ratio there is not a great rationale for delaying treatment, unless the patient’s other eye is healthy and the RVO is not affecting his or her lifestyle.
Another unanswered question is how long therapy may be deferred. Twelve-month data from the BRAVO and CRUISE trials suggest that even when sham-treated patients were allowed to receive open-label ranibizumab after month 6, the visual acuity never equalled those of subjects receiving ranibizumab from the outset.
The relative efficacy of ranibizumab versus grid laser for BRVO has not been fully studied. Although the magnitude of benefit achieved by ranibizumab-treated patients was striking, it is unknown how the BRVO control arm would have fared if these patients were allowed laser therapy from the outset.
Frequent and extended retreatments are likely to be required in patients with CRVO. The mechanisms underlying this requirement are unknown – venous recanalization and/or collateral formation is likely to be present after 2 years and, therefore, peripheral nonperfusion may play a critical role.
Future perspectives [76-81]
As such, ultra-widefield fluorescein angiography may play a role in guiding ranibizumab retreatment and/or modifying therapeutic approach. [76,77]Advances in Doppler OCT technology may also allow additional, noninvasive, quantification of retinal blood flow in these disorders. [78,79] OCT angiography can visualize microvascular abnormalities equally well or better than FA in eyes with BRVO/CRVO.[80/81]
Summary:
- Vein occlusion is potentially blinding disease with various vision threatening complications .Although any of the above mentioned drugs may be used as first line for this condition.
- Anti-VEGF is preferred in eyes with a previous history of glaucoma and younger patients who are phakic.
- Dexamethasone implant (Ozurdex) may be a better choice in patients with recent cardiovascular events and in those who do not favour monthly injections.
- Rescue laser photocoagulation can be done after 3-6 months of therapy to reduce the number of the injection.
- In cases of CRVO/HRVO even after 3 years of follow may require injections, BRVO/TRVO respond well.
- Once the neovascularization develops laser photocoagulation is the treatment of choice.
Reference:
- Hayreh SS, Zimmerman B, Podhajsky P. Incidence of various types of retinal vein occlusion and their recurrence and demographic characteristics. Am J Ophthalmology 1990; 117: 429–41.
- Hayreh SS. Prevalent misconceptions about acute retinal vascular occlusive disorders. Prog Retina Eye Res 2005; 24: 493–519.
- Yau JW, Lee P, Wong TY, Best J, Jenkins A. Retinal vein occlusion: an approach to diagnosis, systemic risk factors and management. Intern Med J 2008; 38: 904–10.
- David R, Zangwill L, Badarna M, Yassur Y. Epidemiology of retinal vein occlusion and its association with glaucoma and increased intraocular pressure. Ophthalmologica 1988; 197: 69–74.
- Hayreh SS, Klugman MR, Beri M, Kimura AE, Podhajsky P. Differentiation of ischemic from non-ischemic central retinal vein occlusion during the early acute phase. Graefes Arch Clin Exp Ophthalmol. 228:201-217, 1990.
- Hayreh SS, Podhajsky PA, Zimmerman MB, Ophthalmology. Natural history of visual outcome in central retinal vein occlusion. 2011 Jan; Epub 2010 Aug 17 (1):119-133.
- Hayreh SS, Rojas P, Podhajsky P, Montague P, Woolson RF. Ocular neovascularization with retinal vascular occlusion-III.Ophthalmology. 1983 May; 90(5):488-506.
- Anon. Baseline and early natural history report. The Central Vein Occlusion Study. Arch Ophthalmol 1993; 111: 1087–95.
- Glacet-Bernard A, Coscas G, Chabanel A, Zourdani A, Lelong F, Samama MM. Prognostic factors for retinal vein occlusion: prospective study of 175 cases. Ophthalmology 1996; 103: 551–60.
- Hayreh SS, Zimmerman MB, Podhajsky P, Alward WLM. Nocturnal arterial hypotension and its role in optic nerve head and ocular ischemic disorders. Am J Ophthalmol. 117:603-624, 1994.
- Keyser BJ, Duker JS, Brown GC, et al. Combined central retinal vein occlusion and cilioretinal artery occlusion associated with prolonged retinal arterial filling.Am J Ophthalmol.1994; 117:308–13.
- McLeod D, Ring CP. Cilio-retinal infarction after retinal vein occlusion.Br J Ophthalmol.1976;60:419–27.
- Paques M, Garmyn V, Catier A, et al. Analysis of retinal and choroidal circulation during central retinal vein occlusion using indocyanine green videoangiography.Arch Ophthalmol.2001; 119:1781–7.
- Schatz H, Fong AC, McDonald R, et al. Cilioretinal artery occlusion in young adults with central retinal vein occlusion.Ophthalmology.1991; 98:594–601.
- Williamson TH. Central retinal vein occlusion: what’s the story?Br J Ophthalmol.1997; 81:698–704.
- Zylbermann R, Rozenman Y, Ronen S. Functional occlusion of a cilioretinal artery.Am Ophthalmol.1981; 13:1269–72.
- Ahmed MAbu El-Asrar, Saba AAl Rashaedand Abdel Galil MAbdel Gader. Anterior ischaemic optic neuropathy associated with central retinal vein occlusion eye(2000)14, 560–562; doi:10.1038/eye.2000.143
- Hayreh SS. Anterior ischemic optic neuropathy. 1. Terminology and pathogenesis.Br J Ophthalmol1974;58:955–63
- Hayreh, Sohan Singh. “NEOVASCULAR GLAUCOMA.”Progress in retinal and eye research2007: 470–485.PMC. Web. 13 Mar. 2015.
- Fong, A.C.O., Schatz, H., McDonald, H.R. et al,Central retinal vein occlusion in young adults (papillophlebitis).Retina.1991; 11:3–11.
- Mendrinos E, Machinie TG, Pournaras CJ. Ocular Ischemic Syndrome.Surv Ophthalmol.2010; 55(1):2–34.
- Sharma S, Brown GC. In:Ocular Ischemic Syndrome.Ryan SJ, Hinton DR, Schachat AP, et al., editors. Elsevier; 2006. pp. 1491–502.
- Furlan A.J.,Whisnant J.P.,Kearns T.P.:Unilateral visual loss in bright light; an unusual symptom of carotid artery occlusive disease. Arch Neurol; 1979;36:675-676.
- Schwab P.J.,Okun E.,Fahey F.L.:Reversal of retinopathy in Waldenström’s macroglobulinemia by plasmapheresis. Arch Ophthalmol;1960;64:515-521.
- Martin SC, Raiz S, Marr JE, et al. Plasma total homocysteine and retinal vascular disease. Eye 2000; 14: 590–3.
- Mohamed Q, McIntosh RL, Saw SM, Wong TY. Interventions for central retinal vein occlusion: an evidence-based systematic review. Ophthalmology. 2007; 114:507–519.
- Squizzato A, Manfredi E, Bozzato S, et al. Antithrombotic and fibrinolytic drugs for retinal vein occlusion: A systematic review and a call for action. Thromb Haemost. 2010; 103:271–276.
- Lazo-Langner A, Hawel J, Ageno W, Kovacs MJ. Low molecular weight heparin for the treatment of retinal vein occlusion: a systematic review and meta-analysis of randomized trials. Haematologica. 2010; Sep; 95(9): 1587–1593.
- Mandelcorn MS, Nrusimhadevara RK. Internal limiting membrane peeling for decompression of macular edema in retinal vein occlusion: a report of 14 cases. Retina. 2004; 24:348–355.
- Opremcak EM, Bruce RA, Lomeo MD, et al. Radial optic neurotomy for central retinal vein occlusion: a retrospective pilot study of 11 consecutive cases. Retina. 2001; 21: 408–415.
- Weizer JS, Stinnett SS, Fekrat S. Radial optic neurotomy as treatment for central retinal vein occlusion. Am J Ophthalmol. 2003; 136: 814–819.
- Weiss JN. Treatment of central retinal vein occlusion by injection of tissue plasminogen activator into a retinal vein. Am J Ophthalmol. 1998; 126:142–144.
- Bynoe LA, Hutchins RK, Lazarus HS, Friedberg MA. Retinal endovascular surgery for central retinal vein occlusion: initial experience of four surgeons. Retina. 2005; 25:625–632.
- McAllister IL, Gillies M, Smithies LA, et al. The central retinal vein bypass study: A trial of laser-induced chorioretinal venous anastomosis for central retinal vein occlusion. Ophthalmology. 2010; 117:954–965.
- Browning DJ,Antoszyk AN. Laser chorioretinal venous anastomosis for nonischemic central retinal vein occlusion. Ophthalmology.1998 Apr; 105(4):670-79.
- Anon. Baseline and early natural history report. The Central Vein Occlusion Study. Arch Ophthalmology 1993; 111: 1087–95.
- Anon. Arandomized clinical trial of early panretinal photocoagulation for ischemic central vein occlusion: the Central Vein Occlusion Study Group. Ophthalmology 1995; 102: 1434–44.
- Anon. Evaluation of grid pattern photocoagulation for macular edema in central vein occlusion: the Central Vein Occlusion Study Group. Ophthalmology 1995; 102: 1425–33.
- The SCORE Study Research Group. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with observation to treat vision loss associated with macular edema secondary to central retinal vein occlusion: the standard care vs corticosteroid for retinal vein occlusion (SCORE) Study Report 5. Arch Ophthalmol. 2009; 127:1101–1114.
- Haller JA, Bandello F, Belfort R Jr, et al. Ozurdex GENEVA Study Group ; Dexamethasone intravitreal implant in patients with macular edema related to branch or central retinal vein occlusion twelve-month study results. Ophthalmology 2011;118:2453–60
- Capone A Jr,Singer MA,Dodwell DG,Dreyer RF and et al ; Efficacy and safety of two or more dexamethasone intravitreal implant injections for treatment of macular edema related to retinal vein occlusion (Shasta study).Retina.2014 Feb; 34(2):342-51.
- Brown DM, Campochiaro PA, and Singh RP et al. Ranibizumab for macular edema following central retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology 2010; 117:1124–33.
- Heier JS and Campochiaro PA et al. Ranibizumab for macular edema due to retinal vein occlusions: long-term follow-up in the HORIZON trial. Ophthalmology. 2012; 119(4):802-809.
- Campochiaro PA, Sophie R, et al. Long-term outcomes in patients with retinal vein occlusion treated with ranibizumab: the RETAIN study. Ophthalmology.2014; 121:209-129.
- www.clinicaltrials.gov/ct2/show/NCT01535261.
- www.clinicaltrials.gov/ct2/show/NCT01396083.
- Brown DM, Heier JS, and Clark WL et al. Intravitreal aflibercept injection for macular edema secondary to central retinal vein occlusion: 1-year results from the phase 3 COPERNICUS study. Am J Ophthalmol. 2013; 155(3):429-437.
- Holz FG, Roider J, and Ogura Y et al. VEGF Trap-Eye for macular oedema secondary to central retinal vein occlusion: 6-month results of the phase III GALILEO study. Br J Ophthalmol 2013; 97:278–8.
- Khurana R. NEWTON study: intravitreal aflibercept injection for previously treated macular edema associated with central retinal vein occlusions. Paper presented at: American Academy of Ophthalmology 2014 Annual Meeting; October 17-21, 2014; Chicago, Illinois
- Alex Yuan,Baseer U. Ahmad,David Xu and et al; Comparison of intravitreal ranibizumab and bevacizumab for the treatment of macular edema secondary to retinal vein occlusion;Int J Ophthalmol. 2014Feb; 7(1): 86–91.
- Epstein DL, Algvere PV, Von WG, et al. Bevacizumab for macularedema in central retinal vein occlusion: a prospective, randomized, double-masked clinical study. Ophthalmology 2012; 119:1184–9.
- Braithwaite T, Nanji AA, Lindsley K, Greenberg PB. Anti-vascular endothelial growth factor for macular oedema secondary to central retinal vein occlusion. Cochrane Database Syst Rev. 2014; 5: CD007325.
- Hayreh SS, Hayreh MS. Hemi-central retinal vein occlusion. Pathogenesis, clinical features, and natural history. Arch Ophthalmol. 98:1600-1609, 1980.
- Duker JS, Brown GC. Anterior location of the crossing artery in branch retinal vein obstruction. Arch Ophthalmol. 107:998-1000, 1989
- Weinberg DV, Egan KM. Seddon JM. Asymmetric distribution of arteriovenous crossings in the normal retina. Ophthalmology. 100:31-36, 1993
- Rabinowicz IM, Litman S, Michaelson IC. Branch venous thrombosis - A pathological report. Trans Ophthalmol Soc UK. 88:191-210, 1968.
- Gutman FA, Zegarra H, Zakov ZN. The natural course of temporal retinal vein occlusion.Trans Am Acad Opthalmol Otolaryngol.1974; 78:178–192.
- Michels RG, Gass JDM. Natural course of temporal retinal branch occlusion. Trans Am Acad Ophthalmol Otolaryngol 1974; 78: 166–77.
- Shilling JS, Jones CA. Retinal branch vein occlusion: A study of argon laser photocoagulation in the treatment of macular oedema.Br J Ophthalmol.1984; 68:196–198.
- Amirikia A,Scott IU,Murray TG,Flynn HW Jr,Smiddy WE,Feuer WJ; Outcomes of vitreoretinal surgery for complications of branch retinal vein occlusion. Ophthalmology2001 Feb; 108(2):372-6.
- Houtsmuller AJ, Vermeulen JA, Klompe M, Zahn KJ, Henkes HE, Baarsma GS, Tijssen J. The influence of ticlopidine on the natural course of retinal vein occlusion.Agents Actions Suppl.1984; 15:219–229.
- Hansen LL, Wiek J, Arntz R. Randomized study of the effect of isovolemic hemodilution in retinal branch vein occlusion.Fortschr Ophthalmol.1988; 85:514–516.
- Osterloh MD, Charles S. Surgical decompression of branch retinal vein occlusions.Arch Ophthalmol.1988; 106:1469–1471.
- Charbonnel J, Glacet-Bernard A, Korobelnik J, et al. Management of branch retinal vein occlusion with vitrectomy and arteriovenous adventitial sheathotomy, the possible role of surgical posterior vitreous detachment.Graefes Arch Clin Exp Ophthalmol.2004; 242:223–228.
- Mester U, Dillinger P. Vitrectomy with arteriovenous decompression and internal limiting membrane dissection in branch retinal vein occlusion.Retina.2002; 22:740–746.
- Rogers S, McIntosh RL, Cheung N, Lim L et al. The prevalence of retinal vein occlusion: Pooled data from population studies from the United States, Europe, Asia, and Australia. Ophthalmology 2010; 117:313 – 319.
- The Branch Vein Occlusion Study Group. Argon laser photocoagulation for macular edema in branch vein occlusion. Am J Ophthalmol 1984; 15; 98(3):271 – 82.
- Scott IU, Ip MS, VanVeldhuisen PC, Oden NL, Blodi BA, Fisher M, Chan CK, Gonzalez VH, Singerman LJ, Tolentino M; The SCORE Study Research Group. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with standard care to treat vision loss associated with macular edema secondary to branch retinal vein occlusion: the standard care vs corticosteroid for retinal vein occlusion (SCORE) Study Report 6. Arch Ophthalmol. 2009; 127:1115–1128.
- Campochiaro PA. Safety and efficacy of intravitreal ranibizumab (Lucentis) in patients with macular edema secondary to branch retinal vein occlusion: The BRVO Study. Paper presented at: Retina Congress 2009; October 4, 2009
- Brown DM, Campochiaro PA, Bhisitkul RB, Ho AC, Gray S, Saroj N, Adamis AP, Rubio RG, Murahashi WY. Sustained benefits from ranibizumab for macular edema following branch retinal vein occlusion: 12-month outcomes of a phase III study. Ophthalmology 2011; 118(8):1594 – 602.
- Efficacy and safety of ranibizumab with or without laser in comparison to laser in branch retinal vein occlusion (BRIGHTER).clinicaltrials.gov/ct2/show/NCT01599650?term=BRIGHTER&rank=1.
- Efficacy and safety of ranibizumab intravitreal injections versus dexamethasone intravitreal implant in patients with branch retinal vein occlusion (BRVO) (COMRADE-B). clinicaltrials.gov/ct2/show/study/NCT01396057.
- Campochiaro PA, Clark WL, Boyer DS, Heier JS, Brown DM, Vitti R, Kazmi H, Berliner AJ, Erickson K, Chu KW, Soo Y, Cheng Y, Haller JA. Intravitreal aflibercept for macular edema following branch retinal vein occlusion: the 24-week results of the VIBRANT study. Ophthalmology. 2015 Mar; 122(3):538 – 44.
- Prager F, Michels S, Kriechbaum K, Georgopoulos M, Funk M, Geitzenauer W, Polak K, Schmidt-Erfurth U. Intravitreal bevacizumab (Avastin) for macular oedema secondary to retinal vein occlusion: 12-month results of a prospective clinical trial. Br J Ophthalmol 2009; 93(4):452 – 6.
- Moradian S, Faghihi H, Sadeghi B, Piri N, Ahmadieh H, Soheilian M, Dehghan MH, Azarmina M, Esfahani MR. Intravitreal bevacizumab vs. sham treatment in acute branch retinal vein occlusion with macular edema: results at 3 months (Report 1). Graefes Arch Clin Exp Ophthalmol 2011; 249(2):193 – 200.
- Prasad PS, Oliver SC, Coffee RE, et al. Ultra wide-field angiographic characteristics of branch retinal and hemicentral retinal vein occlusion.Ophthalmology.2010; 117:780-784.
- Tsui I, Kaines A, Havunjian MA, et al. Ischemic index and neovascularization in central retinal vein occlusion.Retina.2011; 31:105-110.
- T. Schmoll, C. Kolbitsch, and R. A. Leitgeb, "Ultra-high-speed volumetric tomography of human retinal blood flow,"Opt. Express17, 4166-4176 (2009)
- A. S. G. Singh, C. Kolbitsch, T. Schmoll, and R. A. Leitgeb, "Stable absolute flow estimation with Doppler OCT based on virtual circumpapillary scans," Biomed.Opt. Express1, 1047-1059. (2010)
- Suzuki N,Hirano Y,Yoshida M,ad et al;Microvascular Abnormalities on Optical Coherence Tomography Angiography in Macular Edema Associated with Branch Retinal Vein Occlusion. Am J Ophthalmol.2015 Oct, Epub ahead of print.
- Coscas F,Glacet-Bernard A,Miere A,and et al; Optical Coherence Tomography Angiography in Retinal Vein Occlusion: Evaluation of Superficial and Deep Capillary Plexa. Am J Ophthalmol.2015 Oct 14. Epub ahead of print.
- Anon. Argon laser scatter photocoagulation for prevention of neovascularisation and vitreous hemorrhage in branch vein occlusion: a randomized clinical trial. Branch Vein Occlusion Study Group. Arch Ophthalmol 1986; 104: 34–41.